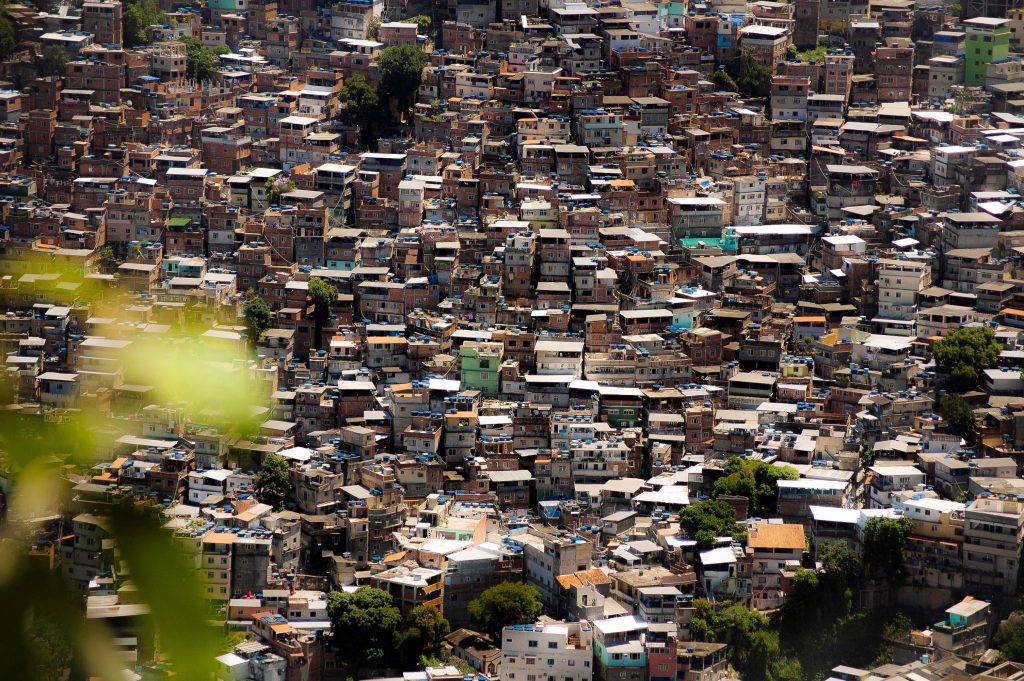
Our world is ‘urbanizing’ rapidly: Two out of every three people are likely to be living in cities or other urban areas by 2050. Do we need to adapt our existing health systems thinking and current models and paradigms? Cities are often unhealthy places to live, but they also offer opportunities for social change, innovation and inter-sectoral solutions, including in health. How to achieve universal access to health in cities? What is the best way to organize health services and the health system in urban settings? How does addressing the impact of urban life impact on the health of urban populations?
When: 15 – 16 October 2019
Where: Espace Jacqmotte, Rue Haute / Hoogstraat 147, 1000 Brussels
The Be-cause health annual conference 2019 links Urban planners and Health professionals. The conference brings together Belgian and international development and health professionals, NGOs and academic researchers, and engages Belgian and international urban planners. The conference will focus on international experiences from low- and middle-income countries. We will also take advantage of Brussels as our host city to showcase urban planning and health experiences and seek exchanges between various international city experiences.
Conference programme
Presentations of the conference
- Day 1: 15 October
- Presentation of Inés Sánchez de Madariaga (bio), Professor of Urban Planning Universidad Politécnica de Madrid, Spain: Cities, Planing, Health and Gender
- Presentation Kristiaan Borret (bio), Master Architect of Brussels, Belgium
- Presentation Guillermo Hegel (bio), Municipal Health Director, Villa Nueva, Guatemala City, Guatemala
- Day 2: 16 October
- Opening Plenary Session: : City experiences on urban health systems unpacked (Track 2)
Rwanda:- A journey to An Integrated, Rationalized, Coordinated, Accessible and Quality Healthcare for the Citizens in the City of Kigali
- Prevention and Control of Non-Communicable Diseases through Mass Campaign in the City of Kigali: preliminary results and lessons
- A proposed Model for the development of medicalized first line health services for the City of Kigali in Rwanda: striving for excellence
- Opening Plenary Session: : City experiences on urban health systems unpacked (Track 2)
- Session A: The challenges of health service delivery in Africa’s mega-cities and urban slums (Track 1)
- Aduragbemi Banke Thomas: Obstetric care in Lagos
- Doreen Tuhebwe: How to improve the design of Reproductive Health (RH) interventions to meet the health access needs of adolescents (15-19 years) living in urban poor settings of Kampala, Uganda
- Félix Vanderstricht: What innovative approachs to progressively integrate the private health centers in the system? The example of the District of Kintambo in Kinshasa
- Session B: Management of urban health systems, a neglected and underexplored reality (Track 2)
- Jean-Marie Ipay: Fourniture des services de santé en milieu urbain état de la situation dans la ville de Gemena en RD Congo
- Daniela Chinnici, & Jean Bosco Kahindo, ULB Coopération Belgium & DRC: Urbanisation et services de santé : le cas des centres de santé médicalisés urbains (CSMU) de Goma, RDC
- Maguelone Vignes, UCL, Metrolab, Belgium: Parcours urbains de soins. Des pratiques aux modèles d’accompagnement des personnes avec des besoins complexes
- Session C: Inequity in urban settings: priority challenge and strategies for better health (Track 3)
- Billy Mwangaza, Etoile du Sud, DRC: La clinique mobile et soins de proximité, une action de lutte contre les inégalités liées a l’acces aux soins a Kintambo
- Pilar Martinez, General Coordinator Médecins du Monde Belgium, DRC: Communes sans viol et le pouvoir au peuple : projet pilote à Bukavu (RDC)
- Pierre Ryckmans, Infirmiers de Rue, Belgium: Présentation Infirmiers de Rue
- Nathalie Annez de Taboada, Health Department, Médecins du Monde, Belgium: Inequity In Urban Settings: Priority Challenge And Strategies For Better Health
- Getting Equal: confronting systems and power
- Session D: One health in cities – linking health and its determinants in urban environments (Track 3)
- Nonvignon Marius Kedote, Health and Environment Department, Regional Institute of Public Health Comlan Alfred Quenum / Ecohealth Chair / University of Abomey-Calavi, Benin: One health in cities – linking health and its determinants in urban environments
- Session E: Embracing complexity of urban governance for health (Track 4)
- Didier Chuy Kalombola, Ecole de Santé Publique de l’Université de Lubumbashi, DRC: The Role Of District Health Management Teams In Urban Stewardship, In Lubumbashi, DR Congo
- Deepika Saluja, Health expert, India: Complex Urban Governance in New Delhi Slums
- Noel Nacoulma, Ministry of Health, Burkina Faso: The complexity of governance of health services in cities – The example of Ouagadougou
- Guillermo Hegel, Municipal Health Director, Villa Nueva, Guatemala City: Developing a Municipal Health Policy – Using the Urban Health Equity Assessment and Response Tool (Urban HEART)
- Session F: How to make it work?: Innovations and solutions in health service delivery in mega-cities and urban slums (Track 1)
- Rachel Hammonds, University of Antwerp /Law and Development Research Group, Belgium; London School of Hygiene and Tropical Medicine, UK: Mothers At Risk – Innovating to improve urban maternal health
- Christine Gilles, CHU St Pierre, Brussels, Belgium: Sexual Assault Referal Center (SARC) Brussels
- Musharrat Jahan, Concern Worldwide – Integrated Urban Program, Bangladesh: Improving Health and Nutrition Status of Urban Extreme Poor
- Jantine Jacobi, UNAIDS, Brussels, Belgium: Cities: the road to success in Ending the AIDS Epidemic Case study on Nairobi
Tracks
The conference held parallel sessions on day 2 around the following six themes :
- Track 1: Urban health service delivery
How can we leverage the urban potential for health service delivery? This question lies at the core of this track. We are interested in sharing innovative ways of organizing health services: how to acknowledge challenges of and effectively use the advantage of urban specificities (scale, proximity, anonymity, …) in order to deliver better care; e.g. how to identify and harness innovation, training and rotation of health staff, providing services at scale. What can we learn from linkages operating within cities through referrals across health providers, and multi-sectoral action such as emergency response teams? This session has also an interest in research/experiences in urban populations’ increased use of (formal and informal) private health services, and the issue of how to engage with private providers who might not recognize public health stewardship.
- Track 2: Urban health systems
Rapid urbanization calls for innovative ways of organizing health systems in cities. A structured effort in that respect is long overdue. Some of the most pressing questions are: does the traditional (WHO) concept of “health districts” hold in urban settings? If not, what is (are) the alternative(s)? If yes, how to adapt them to this specific environment? For instance, would every single urban “district” need its own referral hospital? How to delineate “populations of responsibility” in a urban environment? How to manage the high density of health care providers and their diversity in terms of qualifications and organizational formats? Which are the specificities of care pathways and/or the therapeutic itineraries in urban settings, and how to address them? This session seeks best practices, recent findings on how to capitalize on the range of urban advantages (amongst others in terms of scale, geographical access of services, possibility of choice of healthcare providers and other social services, etc.), and how to adapt to the urban environment with the aim of implementing Primary Health Care (with a focus on some of its key features: stewardship, basic healthcare delivery and multi-sectoral action).
- Track 3.1: Health equity
Income inequality has increased globally and had an impact on the access of urban populations to quality health services. Discrimination and even criminalization prevent ‘key populations’ and minority groups to access essential health services and rights. This session seeks short stories and recent findings engaging with some of the following questions: Which (health) policies can improve access to health in settings marked by vast inequality and inequities? What does community health promotion (or its failure) mean in an (informal) urban setting? Which policies of non-discrimination and access to essential services such as mobility, housing, water and sanitation, etc. determine the health of the city’s diverse populations?
- Track 3.2: Eco-health: linking health and environment
Cities are often unhealthy places to live due to the impact of several factors, such as air-pollution, noise pollution, existence of food deserts, poor quality housing and infrastructure in slum areas, and lack of access to green spaces. This session seeks short stories and recent findings on: How to better link urban planning/ and take advantage of urban scale and geography, innovate upon circular ‘local’ production/economy, and other interventions supporting a healthier environment for urban populations.
- Track 3.3: Ensuring safety in the city
Cities innovate and invest to become “child proof”, accessible, bicycle-friendly, aim to upgrade ‘no-go’ areas with weak (public) service delivery, and city residents campaign against crime and sexual and gender-based violence. This session aims to address various topics related to safety including ways to reduce road traffic mortality, to address high levels of (sexual) violence in urban areas, to manage health hazards of waste management, and overall ways for city governments to plan and coordinate multiple (health and other) stakeholders to improve safety. Can the rising use of surveillance, ‘smart’ cities and artificial intelligence contribute to this goal?
- Track 4: Urban planning & Urban (health) Governance
(Progressive) City governance requires a multi-disciplinary approach to improve urban health embracing the complexity of decision-making and implementing co-governance (collaborative governance) with a multitude of stakeholders and hitherto ignored communities. This session aims to share best-practices and facilitate a debate on how to coordinate health districts under ministry of health and local governments’ public services purview such as water and sanitation, public transportation and housing. What does it take to include health assessments in urban planning and decision-making and to move toward to more coordinated (HealthinAll) policies and better accountability?
The conference is organized by Be-cause health in partnership with Enabel – Belgian Development Agency, Memisa, the Institute of Tropical Medicine (Antwerp), Sensoa, University of Antwerp, Université de Liège, Université Libre de Bruxelles/Ecole de Santé Publique, ULB Coopération and Viva Salud.
Call for stories and abstracts closed!
We have invited individuals to submit short stories or scientific abstracts on recent (research) findings. The conference seeks to exchange on diverse health needs of urban populations (regardless of age, sexual orientation, background), including Sexual Reproductive Health and Rights – SRHR, health responses to existing infectious diseases such as Zika, influenza, HIV, TB, and emerging urban epidemics such as the co-existence of malnutrition and overnutrition/obesity, diabetes and sedentary lifestyles. Read more about the call.
Supported by


























